Clubfoot is a congenital disorder that occurs in 1 out of 1,000 births per year. In newborns, the condition presents as the foot appearing as if it was rotated incorrectly at the ankle*. Several different factors cause clubfoot. Normally, clubfoot occurs due to genetics; however, some environmental factors are a possibility as well. Breech presentation and the position of the baby in a womb can cause clubfoot, as well as certain connective tissue disorders. This abnormality is often noticed during an ultrasound of the pregnancy at the 20th week.
A common treatment of clubfoot is reshaping. This is suggested to be done shortly after a child is born. The foot or feet are put into place and then casted on the legs* for stability. Required check-ups occur once a week to stretch and recast the feet. This process is done for about 5-10 weeks. Afterwards, one more cast is placed on for 3 weeks. Once positioned correctly, a child needs to wear a brace day and night for 3 months. For the next 3 years, while sleeping, the brace must be worn. These steps are taken to prevent the feet from reverting back to its misshapen position.
While this non-surgical approach has been proven very successful, severe cases of clubfoot may require surgery. Clubfoot surgery is usually performed after nine months of age. If surgery is performed, corrective shoes or a brace must be worn for up to a year afterwards as a supplemental measure. Secondary or repeat surgeries may also be needed to correct scar tissue damage as the child grows. In rarer cases, a surgical procedure may be needed as an adult.

One of the most common causes of pain felt in the ankle region is a sprain. When ligaments in the ankle are torn or overstretched, an ankle sprain is likely to occur. There are three types of sprains that may develop: mild, moderate, and severe. In the case of a mild ankle sprain, the ankle is stable. The ligaments, however, are stretched. A moderate sprain consists of one or more ligaments being partially torn, and there’s limited movement. Severe ankle sprains include one or more torn ligaments, the ankle being unstable, and an inability to move the foot.
Ankle sprains are a common occurrence for those who are particularly active in sports. Volleyball, basketball, and soccer are just a few of the types of sports that are prone to producing ankle injuries, including ankle sprains. Many athletes have found that compressing the ankle by wrapping it in bandages is an effective method for helping to prevent injury. Exercising using a balance board has also been found useful for strengthening the ankle and increasing its stability.
If you’re experiencing ankle pain and believe you might have a sprain, it’s highly recommended that you consult with a podiatrist for a proper diagnosis and advised treatment plan.

The pain caused by Morton’s neuroma is typically experienced at the ball of the foot. Many have described the sensation as feeling like they have a pebble stuck in their shoe. Because of this, those with the condition may find walking to be more difficult and uncomfortable. They may also experience a numbing or burning sensation in the foot. One of the most common factors that influence the development of Morton’s neuroma is improper footwear. Those who generally wear tightly fitted shoes or shoes with higher heels are more at risk at getting Morton’s neuroma. Having a foot abnormality may also increase the risk of getting this condition, as it may cause instability, thus adding more pressure onto the nerves of the foot. Certain foot conditions such as bunions, hammertoes, and flat flat feet have also been known to lead to Morton’s neuroma if not treated promptly.
Athletes have a tendency of getting Morton’s neuroma due to repetitive motions and pressure placed on the ball of the foot while running or jumping. Morton’s neuroma may also develop as a result of an injury to the foot.
To learn more about Morton’s neuroma and treatments that work best for your case, consult with your podiatrist.
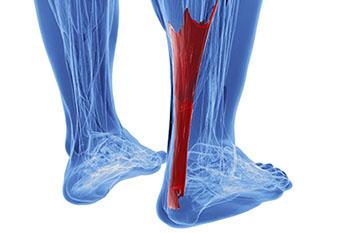
A condition that often results in serious heel pain is known as Achilles tendonitis. This condition may form when the Achilles tendon is damaged as a result of overuse. This particular injury can be very serious, as the Achilles tendon’s main function is to connect the lower half of the calf muscles to the heel bone. If this tendon becomes damaged, it may result in difficulty walking and completing everyday tasks, as well as cause extreme discomfort and pain.
It’s more common for athletes to experience Achilles tendon injuries, as they’re more likely to be participating in activities that would call for repetitive movement, such as running or jogging. This kind of repetitive movement over time is likely to cause stress on the tendon. When athletes abruptly increase their performance level without properly training or warming up their bodies, they may also injure the Achilles tendon, which may lead to inflexibility in the calf muscles.
In order to prevent this kind of injury, it’s suggested to perform stretches—particularly focused on the calf region—about one to three times a day to keep the area flexible. Focusing on building strength in your calves is also advised. If you believe you’ve injured your Achilles tendon, there are some actions you can take to help alleviate the discomfort. Icing and massaging the affected area may help to calm the pain, as well as practicing light stretches.
If you’re having difficulty walking or icing the area does not alleviate the pain, it’s highly advised that you speak with a podiatrist for professional care and an advised treatment plan.
 Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot to continually absorb the full impact of each step someone takes. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot to continually absorb the full impact of each step someone takes. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their Feet. Individuals who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot, and allow you to continue living normally.